
Blog
Testing for COVID-19 beyond the clinic: using wastewater epidemiology to proactively detect outbreaks

March 12, 2020
Our public health systems are reactive. Here’s how we think sewage can help.
Public call to action
Let’s use sewage to map the outbreak of COVID-19 and provide real-time data for governments and communities to get ahead of the crisis.
Current context
The COVID-19 pandemic has led to unprecedented responses from governments around the world. China built two hospitals in ten days, Italy is locked down in an attempt to control the outbreak, and large gatherings all over the US are being canceled while universities move their semesters online. While very important to control the spread of the virus that causes COVID-19, these reactions to an out-of-control situation highlight a critical weakness in our public health systems: they’re reactive. Rather than catching outbreaks early on, we respond after they reach epidemic status and resources are strained.
The US has been particularly slow to roll out diagnostic testing for COVID-19, leaving everyone wondering how big the outbreak really is. At the time of this writing, there isn’t yet agreement between the CDC, state health departments, and local hospitals on which patients are prioritized for testing. This is a problem because the number of confirmed cases matter. Based on these official numbers, cities and states can communicate with the public, declare a State of Emergency, and unlock extra resources and funding. These numbers also inform and validate other decisions, such as canceling events and closing schools to curb the spread of COVID-19.
Problem
All eyes are on this emerging pandemic: emergency resources and funding are being quickly allocated to support research and response, and many individuals and institutions are stepping up and doing their part to curb the spread of the virus. But even in this extreme situation, the data we have to inform our response is reactive and delayed, and doesn’t include everybody who has the disease.
- How are we supposed to get ahead of an epidemic that is changing by the day, when we’re restricted to a subset of data from days, weeks or even months prior?
- How are we supposed to keep our population safe from a spreading virus, when only those with the most severe symptoms can be tested?
These data gaps aren’t unique to the COVID-19 outbreak. In other epidemics, like the U.S. opioid crisis, delays for official data can be up to one or two years, and only the most severely affected, those who overdose, get counted. This leaves us with public health responses designed for yesterday’s epidemics.
Technology
We believe that one key to resolving these public health data crises lie in a place you might not think about: sewage. Sewage contains valuable information on human health, since viruses, bacteria, and chemical metabolites are excreted in urine and stool and provide a readout of an individual’s health status. In some diseases, people excrete viruses before they show symptoms, meaning that sewage can provide an early indicator of disease spread before people start seeking care. The technical term for analyzing sewage as a source of public health information is Wastewater-Based Epidemiology (WBE). And we believe it can help us respond to COVID-19, and more importantly, transform reactive public health systems into proactive ones.
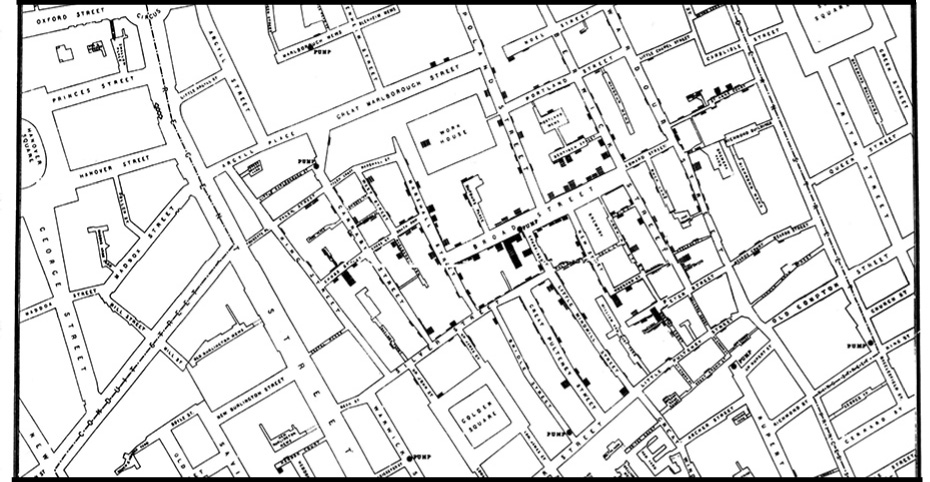
Our mission at Biobot Analytics is to transform wastewater infrastructure into public health observatories. We aim to create a health database that is independent from hospital reporting systems, free from societal biases affecting who can and can’t seek care, and most importantly, rapidly adaptable to new and emerging public health threats. We’ve applied our technology in the US to help public health agencies get ahead of and respond to the opioid epidemic. There’s a strong precedent for our work. The Sewage Analysis Core Group Europe (SCORE) pioneered drug testing in sewage and has been collecting data since 2011 across the European Union. Internationally, wastewater epidemiology has also been used as an early warning detection for another disease: poliovirus. In 2013, researchers in Israel detected an outbreak of poliovirus through their wastewater epidemiology program before any local clinics reported symptoms. Armed with this information, the government targeted vaccination efforts that effectively contained the outbreak. Not a single case of paralysis was ultimately reported.
COVID-19 and the future of public health
There is an incredible opportunity to use this technology to get ahead of and monitor the COVID-19 epidemic. A wastewater epidemiology system that aggregates samples from wastewater treatment plants across the US would provide a real-time map of COVID-19 as it spreads to new places. Without the need for individual testing. Government officials, school administrators, and employers would no longer need to rely on confirmed cases or hospital reporting to make tough decisions like enforcing work from home policies. By empowering decision makers to act earlier, we can flatten the curve, which can make the difference between a healthcare system collapsing or not. In places where the disease is rampant, wastewater epidemiology can track the effectiveness of interventions and the wind-down period of the outbreak. Widespread longitudinal testing will give us an early warning next time the coronavirus emerges, if it does indeed have a seasonal cycle.
Most valuable, perhaps, is that a permanent wastewater epidemiology infrastructure across America and major cities around the world will enable us to be proactive in our global response to thwart the next infectious disease outbreak before it becomes an epidemic.
Written by Biobot Analytics
Biobot provides wastewater epidemiology data & analysis to help governments & businesses focus on public health efforts and improve lives.





